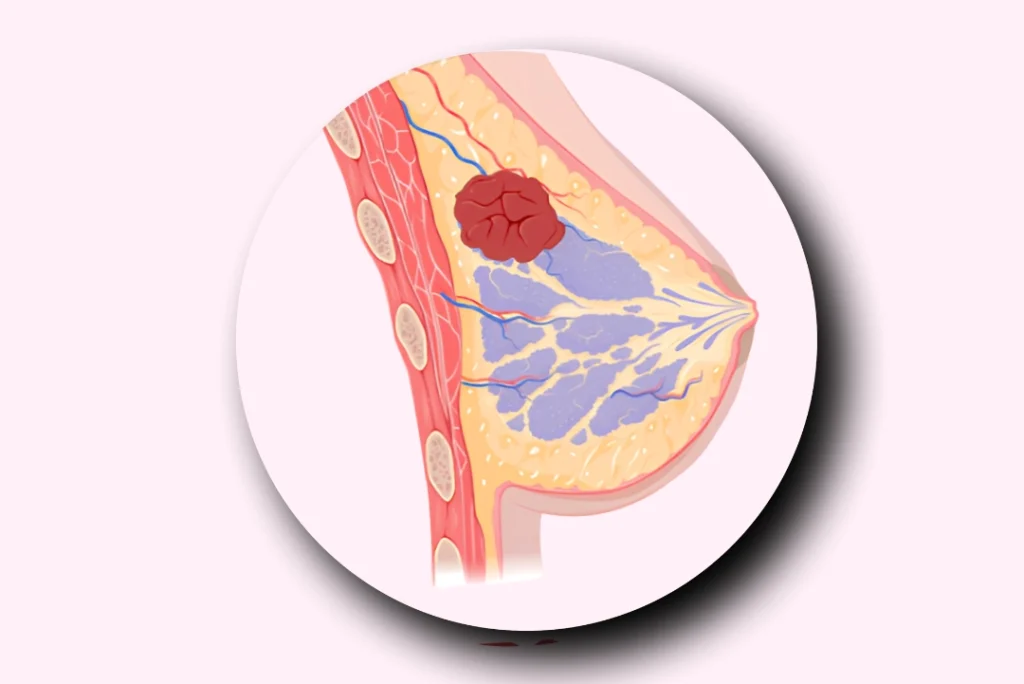
HER2-positive breast cancer is a type of breast cancer characterized by the overexpression of the HER2 (human epidermal growth factor receptor 2) protein. This protein promotes the growth of cancer cells, and its overproduction leads to more aggressive cancer. Approximately 20% of breast cancers are HER2-positive, making this an important subtype to understand and treat. Fortunately, targeted therapies have transformed the outlook for patients, offering effective HER2-positive cancer treatment options.
Understanding HER2-Positive Breast Cancer
The HER2 protein, found on the surface of breast cells, plays a crucial role in regulating cell growth. In HER2-positive breast cancer, mutations cause an excess of this protein, leading to rapid cell division and tumor growth. This type of cancer tends to be more aggressive than other forms of breast cancer but responds well to targeted therapies designed to block the effects of HER2.
HER2-positive breast cancer can occur in any stage of breast cancer, including Stage 4 HER2-positive breast cancer, where cancer has spread to other parts of the body. Understanding the implications of HER2 overexpression is crucial for developing an effective treatment plan.
HER 2 Positive Cancer Treatment
HER 2 positive cancer treatment primarily revolves around targeted therapies, which specifically inhibit the HER2 protein. The most common treatment options include:
- Trastuzumab (Herceptin): This is a monoclonal antibody that binds to HER2, preventing cancer cells from receiving growth signals. It’s often used in combination with chemotherapy.
- Pertuzumab (Perjeta): Another monoclonal antibody that works alongside Herceptin, enhancing its effectiveness.
- Ado-trastuzumab emtansine (Kadcyla): A targeted drug that combines trastuzumab with a chemotherapy drug, delivering it directly to cancer cells.
Chemotherapy, radiation, and surgery are also part of the treatment plan, particularly in advanced cases like Stage 4 HER2-positive breast cancer. The combination of targeted therapies and traditional treatments helps slow down cancer progression and improves survival rates.
Side Effects of HER2 Treatment
Like all cancer treatments, targeted therapies for HER2-positive breast cancer come with potential side effects. Understanding and managing these side effects is an essential part of the treatment journey. Some common side effects of HER2 treatment include:
- Fatigue: One of the most common side effects, affecting daily activities.
- Nausea and vomiting: Often a result of chemotherapy combined with HER2 inhibitors.
- Cardiac issues: Targeted therapies like trastuzumab and pertuzumab can sometimes lead to heart problems. Regular heart monitoring is crucial during treatment.
- Hair loss: Another common side effect, particularly when chemotherapy is involved.
- Low blood cell counts: This can increase the risk of infection and fatigue.
It’s essential to maintain regular communication with your healthcare team to manage these side effects and ensure the effectiveness of your treatment.
Stage 4 HER2 Positive Breast Cancer
Stage 4 HER2 positive breast cancer, also known as metastatic breast cancer, means that cancer has spread beyond the breast and nearby lymph nodes to other parts of the body, such as the bones, liver, or brain. This stage of breast cancer is considered incurable, but treatment options are available to manage symptoms, prolong life, and maintain quality of life.
Targeted therapies have significantly improved outcomes for patients with Stage 4 HER2 positive breast cancer. While complete remission may not always be possible, these treatments can effectively slow down the spread of cancer and reduce tumor size. Patients often receive a combination of targeted therapy, chemotherapy, and possibly radiation therapy, depending on the location and extent of metastasis.
Importance of Early Detection
While treatments for HER2-positive breast cancer have greatly improved, early detection remains one of the most critical factors in ensuring a successful outcome. Regular mammograms, self-exams, and awareness of symptoms can lead to earlier diagnosis, allowing patients to begin HER2-positive cancer treatment sooner. Symptoms to watch for include:
- Lumps in the breast or underarm area
- Changes in the size or shape of the breast
- Nipple discharge, particularly if it’s clear or bloody
- Pain or discomfort in the breast or nipple area
Early intervention is key to reducing the spread of cancer and improving long-term outcomes, particularly before the cancer reaches advanced stages like Stage 4 HER2-positive breast cancer.
What Makes HER2-Positive Breast Cancer Unique?
HER2-positive breast cancer differs from other forms of breast cancer due to the overexpression of the HER2 protein, leading to faster growth and a higher risk of recurrence. However, it also responds uniquely to treatments that target HER2, which are not effective in other types of breast cancer. This means that HER2-positive cancer treatment is highly specialized and focuses on therapies that inhibit HER2, such as trastuzumab, pertuzumab, and newer agents like neratinib.
In contrast, hormone receptor-positive breast cancer or triple-negative breast cancer requires different treatment strategies. This specificity is why it’s essential for patients to receive a thorough diagnosis to determine their cancer type, ensuring the most effective treatment plan.
Conclusion
With advances in HER2-positive cancer treatment, the prognosis for patients has improved dramatically. Whether diagnosed in the early stages or with Stage 4 HER2-positive breast cancer, patients now have access to therapies that target the underlying causes of their disease. Early detection, understanding the risks, and working closely with a knowledgeable healthcare team are critical components of managing this aggressive form of breast cancer.
As treatments continue to evolve, ongoing research holds the promise of even better outcomes for patients with HER2-positive breast cancer. By staying informed and proactive, patients can make empowered decisions that support their long-term health.