Breast cancer disparities remain a pressing issue, highlighting gaps in diagnosis, treatment, and survival rates across different racial and ethnic groups. These disparities reveal not only the differences in breast cancer incidence and mortality rates but also underline the role of social, economic, and healthcare access factors. Addressing breast cancer disparities is critical to ensuring equitable healthcare and improving outcomes for all women. This blog will delve into the factors contributing to breast cancer disparities, how breast cancer impacts different races, and why addressing these disparities is essential.
Breast Cancer Disparities: A Multifaceted Issue
Understanding Disparities in Breast Cancer Incidence and Outcomes
Breast cancer is most common in what race? While breast cancer affects women of all races, incidence rates and outcomes vary significantly. White women have higher overall incidence rates; however, Black women tend to be diagnosed at younger ages and often at more advanced stages, resulting in higher mortality rates. This contrast sheds light on significant breast cancer disparities that affect survival outcomes and quality of life.
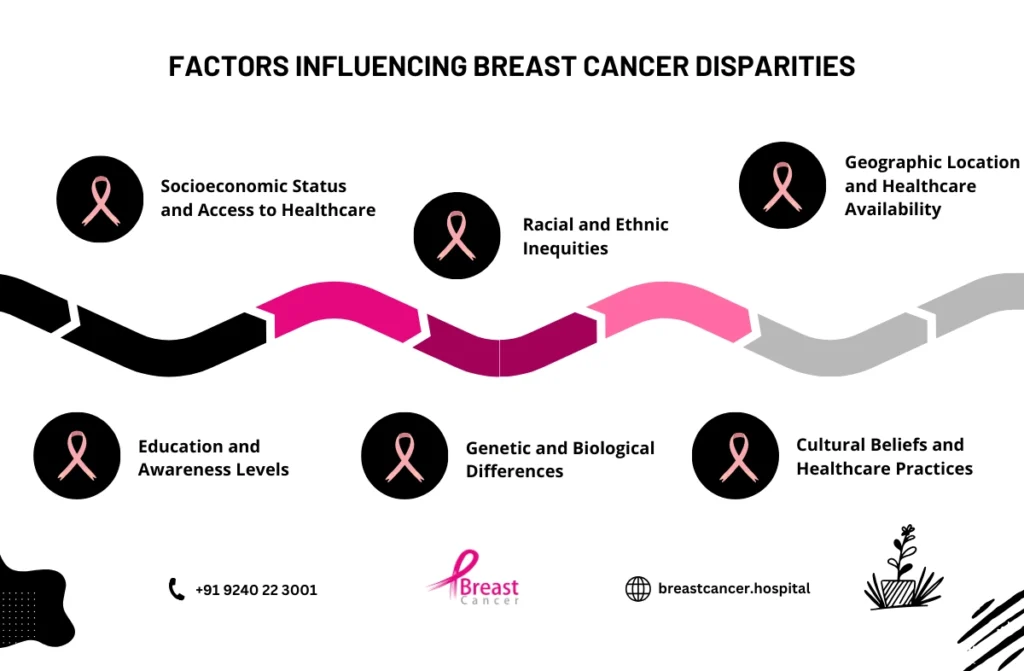
Several factors contribute to these racial disparities in breast cancer. Socioeconomic status, healthcare access, genetic predispositions, and cultural beliefs all play a role. For instance, Black and Hispanic women may face barriers to early detection and high-quality treatment due to limited access to healthcare or financial resources, which can delay diagnosis and hinder treatment outcomes.
Breast Cancer by Race: How Different Communities Are Affected
When examining breast cancer by race, it’s clear that the impact is uneven across populations. White women tend to have a higher incidence of breast cancer overall, yet Black women face the highest mortality rates from the disease. This discrepancy is largely due to differences in healthcare access, insurance coverage, and systemic inequities that impact treatment options and outcomes.
Racial disparities in breast cancer also become evident in the diagnosis of more aggressive breast cancer subtypes. Black women are more likely to develop triple-negative breast cancer (TNBC), a particularly aggressive form with fewer treatment options. These disparities are a reminder of the systemic barriers that can influence disease outcomes and emphasize the need for targeted research and resources to address specific community needs.
Barriers to Equal Treatment: Factors Influencing Breast Cancer Disparities
Socioeconomic Status and Healthcare Access
One of the most significant contributors to breast cancer disparities is socioeconomic status. Income and education levels often correlate with access to health resources, including regular mammograms and follow-up care. Women from low-income communities may lack the means to afford routine screenings or face challenges in accessing specialized breast cancer care facilities, particularly if they live in rural areas.
Healthcare access disparities also affect minority groups disproportionately. In the United States, Black and Hispanic women are less likely to have private health insurance, which can impact their ability to seek early detection and advanced treatment options. Addressing these financial and logistical barriers is key to improving breast cancer outcomes for all.
Biological Differences in Breast Cancer
The prevalence of certain breast cancer types also varies by race, contributing to breast cancer disparities. Black women, as mentioned, are more likely to develop triple-negative breast cancer, an aggressive subtype that lacks hormone receptors targeted by many standard treatments. This subtype requires alternative approaches, but access to specialized treatment can be limited in under-resourced communities.
These biological differences underscore the importance of inclusive research and personalized treatment plans. Investing in research that considers racial differences in breast cancer biology can help improve targeted treatments and ultimately reduce mortality rates in minority populations.
Social and Cultural Factors Impacting Breast Cancer Screening and Treatment
Cultural beliefs, language barriers, and societal stigma also play roles in creating breast cancer disparities. For some communities, discussing health concerns openly is less common, and stigmas around cancer can delay or prevent individuals from seeking early diagnosis. Additionally, language barriers and limited health literacy can create misunderstandings about screening importance and treatment options, ultimately impacting adherence to recommended care.
Community-based outreach programs and culturally sensitive education can help bridge these gaps by providing accessible information and fostering trust in healthcare providers. Empowering patients through culturally appropriate communication can improve early detection rates and encourage treatment adherence.
Racial and Ethnic Groups Affected by Breast Cancer Disparities
Different racial and ethnic groups face unique challenges when it comes to race and cancer diagnosis and treatment. These challenges can impact survival rates and the effectiveness of treatment.
- African American women: They are diagnosed with breast cancer at a younger age and with more aggressive types of cancer, such as triple-negative breast cancer. This form of cancer is more difficult to treat, leading to poorer outcomes.
- Hispanic women: While the incidence rate of breast cancer is slightly lower in Hispanic women compared to white women, their survival rate is lower. Cultural barriers, language, and access to healthcare contribute to this disparity.
- Asian American women: Asian women face unique challenges, particularly related to cultural beliefs about healthcare. These challenges can lead to delayed diagnosis and treatment, contributing to disparities in breast cancer outcomes.
- Native American women: This group faces the highest rates of late-stage race andm cancer diagnosis. Limited healthcare infrastructure and access to screenings in rural areas contribute to these disparities.
Addressing Breast Cancer Disparities: Steps Toward Equity
Raising Awareness and Encouraging Early Screening
Promoting awareness around breast cancer disparities is a critical first step in reducing inequities. Encouraging early screening among high-risk populations, particularly in communities with limited healthcare access, can lead to earlier detection and improved survival rates. Public health campaigns tailored to diverse racial and ethnic communities can address knowledge gaps and emphasize the importance of mammograms and regular check-ups.
Additionally, healthcare providers play a role in promoting awareness by educating patients about breast cancer risks and addressing misconceptions about the disease. By fostering open communication and addressing concerns unique to each patient’s background, healthcare professionals can build stronger relationships that encourage proactive health management.
Expanding Access to Quality Care and Resources
Improving access to quality healthcare is essential to reducing racial disparities in breast cancer. Financial assistance programs, transportation services, and partnerships with community clinics can help mitigate logistical barriers that prevent individuals from seeking timely care. Expanding insurance coverage and offering low-cost mammography screenings in underserved areas are also effective ways to make early detection accessible to more people.
Hospitals and health organizations should also consider implementing diversity training programs to ensure culturally sensitive care for patients from different racial backgrounds. By creating a more inclusive healthcare environment, providers can reduce potential biases and improve patient trust and satisfaction.
Investing in Research for Inclusive Treatment Options
To address breast cancer disparities effectively, research must be inclusive and representative of all racial groups. Studies that focus on breast cancer by race can provide critical insights into unique risk factors and biological differences, enabling the development of more effective and personalized treatments.
Pharmaceutical companies, researchers, and public health agencies should prioritize funding for studies that examine racial and ethnic disparities in breast cancer. By understanding the genetic and environmental factors that contribute to these disparities, researchers can develop targeted therapies that improve outcomes for minority populations.
Breast Cancer Disparities Statistics
Breast cancer disparities are evident when we look at the statistics. While breast cancer statistics by race is common across all racial and ethnic groups, the outcomes and experiences vary greatly. In fact, studies show that certain racial groups face higher risks, more advanced stages of the disease at diagnosis, and lower survival rates.
- Breast cancer by race: African American women are diagnosed with breast cancer at a higher rate than their white counterparts at a younger age. Additionally, they often present with more aggressive forms of breast cancer, such as triple-negative breast cancer.
- Racial disparities in breast cancer: Native American, Hispanic, and African American women have historically shown lower breast cancer survival rates compared to Caucasian women, even though the incidence rate is similar or lower in these groups.
- Breast cancer is most common in what race? While breast cancer is prevalent across all races, it is more commonly diagnosed in white women. However, Black women face a greater risk of aggressive forms of the disease, leading to higher mortality rates.
Key statistics that reflect cancer disparities include:
- African American women are 40% more likely to die from breast cancer statistics by race than white women.
- Hispanic women have a 17% lower chance of survival compared to non-Hispanic white women.
- Native American women have lower survival rates due to delayed diagnosis and limited access to healthcare.
Disparities in Breast Cancer Deaths
The disparity in breast cancer deaths is another critical area of concern. Even though breast cancer statistics by race affects women of all backgrounds, the survival rates vary significantly based on factors such as race, access to care, and socioeconomic status.
- Breast cancer deaths by race: African American women, for example, are more likely to die from breast cancer, even though their rates of diagnosis are slightly lower than white women. This disparity is largely attributed to the later stages of diagnosis, as well as the aggressive nature of the cancer when it is detected.
- Racial disparities in breast cancer survival: Research has shown that African American women are more likely to be diagnosed at a later stage, when treatment options are more limited, and the prognosis is poorer. This is often due to barriers in healthcare access, such as inadequate insurance, lack of early screening, and limited access to quality healthcare providers.
- Socioeconomic factors also play a major role in survival rates. Lower-income women, especially in minority groups, often lack access to preventive care, early screening, and advanced treatments.
Conclusion
Breast cancer disparities remain a significant barrier to equitable healthcare, affecting diagnosis, treatment, and survival rates across racial and socioeconomic lines. Addressing these disparities is essential to ensuring that every individual has access to the best possible breast cancer care, regardless of their background or financial status. Understanding the impact of breast cancer by race, raising awareness, and prioritizing research are crucial steps in reducing racial disparities in breast cancer.
Improving healthcare access and fostering inclusive research can bridge gaps and enhance treatment outcomes for all individuals. By prioritizing equity in healthcare, we can create a future where breast cancer survival is no longer determined by race, location, or socioeconomic status. Taking action today can make a lasting difference in the lives of countless women affected by breast cancer disparities.




